動画タイトル
がんの早期発見と予防(CME) – How to Detect Cancer Early Before it Spreads by Peter Attia, MD
がんになるといことは、極論「バッド・ラック(運が悪かった)」ということ。たばこを吸わなくても、生活習慣を改善しても、なるときはなる、何故ならがん発生のメカニズムは「体細胞変異」だから。人の自然免疫T細胞はがんの抗原を見つけてやっつけるのが仕事。年を重ねると免疫機能は衰える、すると変異したがん細胞を全て「駆除」することは難しくなり、「綱引きゲームはがん優勢」になり、そしてがんは指数関数的に増殖する・・・
(フルテキストと語彙は最後にあります。)
目次
Topics covered in this video: How to Detect Cancer Early – Before it Spreads:
- Intro to Peter Attia, MD, and Outlive
- Summary of most common causes of mortality 死因ランク
- The 4 key chronic diseases: Cardiovascular, Cancer, Neurodegenerative, and Metabolic 四つの重要な慢性疾患「心血管、がん、神経変異、メタボリック」
- “Healthspan” vs Lifespan ”健康”寿命
- Medicine 2.0 vs Medicine 3.0
- Life expectancy changes over time 寿命の変化
- Countries that focus more on prevention? Single-payer insurance?
- Kyle Allred shares his cancer diagnosis
- Dr. Attia’s approach to cancer with his patient
- What is driving cancer: current understanding
- Somatic mutations and “bad luck”
- Very early and aggressive cancer screening rationale
- Metastatic cancer treatment remains largely unsuccessful
- Checkpoint inhibitors and other immunotherapy
- Inside the body vs outside the body cancers
- The power of direct visualization of colon and polyps
- Colon cancer screening specifics: age, frequency, etc.?
- Bowel prep for colon importance and tips
- Colonoscopy risks and upper endoscopy (Barrett’s esophagus)
- Pills for colon bowel prep (Sutab) vs liquid prep
- Tips when choosing a GI specialist for a colonoscopy
- Blood tests for colon cancer screening (FOBT and Cologuard)
- How quickly can colon cancer develop?
- Breast cancer: Peter Attia’s approach (age, modalities, etc.).
- “Stacking” screening modalities for breast cancer
- Mammography strengths and weaknesses (dense breast tissue)
- MRI and ultrasound for breast screening pros/cons.
- Stagger cancer screening modalities?
- Level 1 medical evidence and costs
- Genetic testing for breast cancer vs family history?
- Liquid biopsy for cancer detection
- The future of liquid biopsies for cancer screening
- Metal detector analogy for sensitivity vs specificity
- Prostate cancer: Dr. Attia’s approach to PSA, imaging, and 4K tests
- Multiparametric MRI for prostate screening
- Empowering ourselves as patients with knowledge
- Incidence of prostate cancer. 80% in men of age 80?
- Lung Cancer increasing in never smokers
- Full body MRI screening for cancer?
- Aneurysm on MRI
- Exercise and cancer prevention?
- Possible impact of stress, immunity decline, etc.
- Other cancer screening: cystoscopy, lung, and more.
- Genetic testing recommended?
- Final thoughts on EARLY cancer screening and the future
- Where to find more of Peter Attia, MD

💰通常90分15,000円 → 初回のみ半額7,500円
初回カウンセリングでは、現在の課題や目標を一緒に整理します。
単発のご相談だけでも歓迎しています。
Full Story
Full Story
- Intro to Peter Attia, MD, and Outlive
I’m excited to be here with Dr Peter attia who is perhaps the leading expert on communicating
what things are we most likely to die from /how can we prevent them
and how can we use data-driven approaches to optimize our health now and for as many years as possible
Dr Attia’s medical degree is from Stanford /he trained at Johns Hopkins general surgery
and he also trained as a Surgical Oncology fellow at the National Cancer Institute
he’s the founder of a website called early medical /the host of a popular podcast called the drive and
the author of outlive a fantastic book just published
we’ll discuss several topics from it
Dr Attia welcome
/ thank you so much for having me
we’ll get to strategies and specific tools for optimizing our health and avoiding cancer and disease in a minute
- Summary of most common causes of mortality 死亡原因
but first for someone watching this
what are they most likely to die from and why is that so important to know
given that we’re watching this in 2023 and not / you know/ 1823 /
it looks a lot different than it did(looked) historically at least for most of our evolutionary past /
today we’re most likely to die from things that I call slow deaths
/ whereas for virtually事実上 all of our existence /we were more likely to die from Fast deaths
fast deaths think of things like infections and Trauma /
but today we’re going to die from chronic disease most likely
and those chronic diseases / in rank order [ランキング]順に approximate
- The 4 key chronic diseases:
- Cardiovascular, 心臓血管疾患
- Cancer,
- Neurodegenerative, 神経変性疾患 and
- Metabolic
cardiovascular and cerebrovascular脳血管の disease /
cancer /
and neurodegenerative disease
we also have a whole host of 数多くの metabolic diseases
that while they don’t directly result in loss of life at as high a frequency頻発
contribute overwhelmingly to the suite of 一連の chronic diseases I mentioned above
so things like type 2 diabetes /non-alcoholic fatty liver disease /insulin resistance
they don’t show up directly on death certificates that often
but their contribution to those other three is enormous
so collectively I call those The Four Horsemen of death
Four Horsemen of the Apocalypse
《the ~》黙示録の四騎士◆新約聖書の記述において、世界の終わりに現れるとされる存在。
- “Healthspan” vs Lifespan
and in your book you talk a lot about the difference between lifespan and health span
can you review what that difference is
sure lifespan is I guess the easier of the two to understand because it’s quite binary 双対
/you know/ you’re either alive or you’re dead and /you know/ you’re breathing or you’re not
/ so / lifespan is essentially the length of your life and a part of longevity寿命
is asking the question can we extend that period of time
/ but an often overlooked component of longevity it’s Health span
and health span is quality of life
and that’s much harder to Define
because it’s /you know/ medical definition is relatively useless
the medical definition of Health span is the period of time for which we are free from disability and disease
but /you know/ I think most people would agree that
even as you age
even if you do so without disability or disease
your physical and cognitive performance for example deteriorate
also your emotional health which doesn’t really fit into a disability and disease standpoint
unless
of course we’re talking about it rising to the level of true mental health
will clearly contribute to your quality of life as well
so quality of life at least around these three areas of physical, cognitive and emotional health contribute at least as much and probably more to the overall concept of longevity
- Medicine 2.0 vs Medicine 3.0
another concept that you mention a lot in your book is this difference between medicine 2.0 as you call it
kind of the status quo 〔現在の〕体制 what we have right now versus medicine 3.0
something that you talk about with your patients and practice yourself
/ could you give us kind of an overview of the difference between these two
sure medicine 2.0 is the system of medicine that we evolved to obviously for medicine 1.0
in the latter part or middle part of the 17th century with the kind of elucidation 解明 of the scientific method
all the way into the latter part of the 19th century with the development of the light microscope
and ultimately into the early 20th century with the development of antibiotics antimicrobial agents and of course vaccines
and what medicine 2.0 then did was allow us to basically dramatically cull(殺)処分する fast death
- medicine 1.0
- the latter part or middle part of the 17th century
- with the elucidation 解明of the scientific method
- medicine 2.0
- the latter part of the 19th century
- with the development of the light microscope
- medicine 3.0
- the early 20th century
- with the development of antibiotics antimicrobial agents and vaccines
- Life expectancy changes over time
so we took fast death which again for all of our existence for /you know/ millions of years was effectively what was going to end our lives
and that meant we were going to die somewhere in our 30s to 40s typically
if we didn’t if we managed to survive childhood
and infant mortality was through the roof
so mothers are /you know/ based dying at an alarming rate every time they’re giving birth to a child
it basically allowed us to escape that and get to the point where we are now primarily dying of these chronic diseases that we talked about a minute ago
so medicine 2.0 says look we’re going to still use the same Playbook to go after those diseases different side of diseases
so it’s /you know/ we’ve hit it out at ~を激しく攻撃する the park with infectious diseases communicable diseases and Trauma
so now let’s ask the question
what if we take the same Playbook and apply it to chronic diseases
The Playbook being you come up with a diagnosis
you treat pharmacologically surgically or however once that disease is present
and I don’t need to State the obvious当然の[分かりきった]ことを言う[述べる] here
but that approach has been largely unsuccessful against chronic diseases
chronic diseases are not as amenable to〔治療方法など〕に適している that strategy
and when you apply the tactics and strategy from Med 2.0 to the current Suite of problems
we have not been very successful
and it’s so Stark 〈古〉〔死体が〕硬直したthat if you take a look at the life expectancy of people 120 years ago
and you strip out剥ぎ取る the top eight infectious and communicable diseases
you realize it’s almost the same as it is today
so yes it’s true we have doubled life expectancy
but that has come almost exclusively through the lens of those early successes of medicine 2.0
so the question then is what is medicine 3.0 and why would it be different
and it basically comes down to~に及ぶ、~に行き着く a fundamental philosophical shift around the acceptance of prevention and very very early prevention
- Countries that focus more on prevention? Single-payer insurance?
many people watching this are going to be watching from the United States and
they’re familiar with this medicine 2.0 Paradigm where we like
you said we wait till disease happens and then we we try to treat it
are there any countries or places that have this better than we do
and are more on the path towards medicine 3.0 that you’re aware of
yes although only sort of slightly right
so there are definitely countries in Europe that have a bit more of a preventive strategy
it’s largely a result of their Health Care system
so the U.S Healthcare System is not really well geared up / for ~の準備をするmedicine 3.0
in fact the the the the transition to Medicine 3.0 will be harder in the U.S than in many other countries
and one of the reasons for that is just a structural reason that has to do with the financial incentives and remuneration for how health care is compensated
so in a system like ours where the majority of care especially early in life is private not public not single-payer
the financial incentive is really geared towards /you know/ getting paid to treat disease
now I’m not advocating for a Single Payer system because I could argue with equal veracity真実性
why a single-payer system is usually quite unsuccessful as well
so it really probably needs to be a hybrid
but here is where the single-payer system does get a nod which is
it is easier to tweak自動車や機器の機能を改善するために〕微調整[マイナーチェンジ]する the incentives towards prevention because you don’t have the financial incentive to provide delayed treatment
in other words
in a single-payer system the payer which is the government owns the risk of disease for the duration of your life
conversely in a system like ours Health Care is very portable
so who’s your insurance carrier right now
Moda which is just a local one in here in Oregon
okay so I /you know/ can’t speak to them specifically
but let’s just assume /you know/ they might only own a life
meaning own the risk of that person’s life for /you know/ five or six years
so are they really interested in putting the time effort and resources into prevention
when you’re in your 20s and 30s if those things are only going to reap rewards〔努力などに対する〕報酬を得る
when you’re in your 50s 60s 70s or 80s
it’s very unlikely /
again this is one of many of the structural challenges with transitioning from medicine 2.0 to 3.0
but to your question
countries that have a single-payer system have a much easier time making that transition
because if you’re in Canada or the UK or Australia or many of the European countries
/ /you know/ the government is effectively backstopping your health care well
- Kyle Allred shares his cancer diagnosis
I want to get into / one of the horsemen that you mentioned
/ cancer and this is a topic of particular interest to me
because I was diagnosed with a type of cancer called Hodgkin lymphoma about six months ago
fortunately it has a very high survival rate and a complete remission rate in someone my age
so it’s likely that the chemotherapy that I’ll be finishing up soon will be the the only treatment I need for this
but my personal interest in screening for cancers is higher than it was before
because I’ve been reminded firsthand〔情報の入手などが〕じかに、直接に
that cancer does /you know/ can and does happen in 40 year olds like me without other medical problems or a strong family history of cancer
so let’s hear about your approach to cancer again within this kind of medicine 2.0
what we have now and what you would like to see and what you recommend with your patients regarding cancer
- Dr. Attia’s approach to cancer with his patients
well each of the horsemen has a slightly different Playbook to go down the medicine 3.0 route
and truthfully when it comes to cardiovascular disease
it’s the easiest of the lot
because we have both the greatest understanding of what causes it
and the greatest set of tools to prevent it
so in other words
if we really know what’s driving it
/you know/ we could go down that rabbit hole in detail
and we happen to have all the tools in the world pharmacologically and non-pharmacologically to lay down〔~を〕横たえる the prevention Gauntlet〔中世のよろいの〕こて◆手を保護するための装甲手袋 decades in advance
- rabbit hole
Oxford Languagesの定義 · 詳細
used to refer to a bizarre〔言動・外観・出来事・性質などが普通ではなくて〕奇妙な、奇怪な、一風変わった, confusing, or nonsensical〔思考・言動などが〕理にかなっていない、ばかげた、無意味な situation or environment, typically one from which it is difficult to extricateから抜け出す oneself.
let’s take Alzheimer’s disease
we actually have quite a strong sense of what the drivers are
some of them are not modifiable they are genetic
but many of them are highly modifiable and
we have some sense of what tools to use therefore to prevent it
unfortunately we have very few tools to treat it once it’s present
- What is driving cancer: current understanding
so cancer occupies kind of a unique place in that landscape in that
we frankly have hands down 断然 the least understanding of what is driving it
we know a few things right
we know that smoking dramatically increases the risk of cancer
but I’m willing to guess you were not a smoker
correct
we know that the second leading environmental or modifiable risk factor for cancer is obesity
which really isn’t about obesity
it’s probably much more about the internal environment that tracks with跡をたどる[追う] obesity
namely hyperinsulinemia《医》高インスリン血(症) and inflammation
and again I’m guessing that that was not necessarily risk factors for you as well
so what that leaves us with is at the end of the day cancer is very much about bad luck
- Somatic mutations体細胞変異 and “bad luck”
in other words cancer is a condition where the majority meaning 95 percent arise from what are called somatic mutations
so these are not mutations in genes that you acquired from your parents
these are genes that you inherited that were completely normal
but over the course of your life and again in your life
being so short to date that you’ve already had this bad luck of acquiring enough mutations to drive a cancer
and the reality of it is
if we were sitting here five years ago having this discussion before you had cancer
I could have told you everything under the sun to do to minimize that risk and maybe it would have
but ultimately you could have still come down with cancer
so why am I saying all of this
- Very early and aggressive cancer screening rationale
well I’m saying all of this because what it does is
it calls to our attention another tool that is essential in our fight if you will against cancer
and that is the tool of very early and aggressive cancer screening now
that’s a highly controversial topic and we can I’m happy to talk about all the controversies
but the rationale is unambiguously明確に、明らかに straightforward / based on the following
there is no example that I am aware of
a cancer where the odds of eliminating it go down as the tumor burden goes up
meaning the fewer cancer cells a person has in their body the more effective the treatment
and I think the simplest explanation for this is that
the more cancer cells you have the more heterogeneous the population of cancer cells
and the more heterogeneous the mutation burden
and as that burden of mutation Rises you have greater and greater chances for escape
meaning you provide a systemic treatment like chemotherapy
and you have a greater and greater likelihood that some cancer cells will actually be able to evade the therapy and go on to develop a new population of cancer cells that will be resistant to treatment
and so /you know/ the the easiest way to look at this is
just to look at colon cancer or breast cancer for which we have so much data
and I write about both of these in the book where
if you take a patient with stage three colon cancer for whom you resect the colon
and you resect the lymph nodes around
but there is no gross or visible spread of the disease say to the liver or other organs
and you give that patient a chemotherapy regimen
their survival in five years is very high /you know/ 60 70 percent
if you take a group of patients with metastatic colon cancer
so the exact same patient but now the cancer is also in the liver
so you can actually see it and you give them the exact same chemotherapy
none of them will be alive in five years
again similar examples with with breast cancer and other forms of cancer
so regardless of how much we do individually to reduce our risk of cancer
and we can talk about all of those things
the importance of exercise nutrition sleep probably and clearly mitigating factors like insulin resistance and smoking
at the end of the day結局は[のところ] we are still every one of us susceptible
and therefore I think it’s imperative不可避 that we at least consider what very early screening does to give us a chance to
if we do have cancer , fight it with the smallest burden
- Metastatic cancer treatment remains largely unsuccessful
possible and another thing that you mentioned in your book that convinced me
on the importance of early and aggressive screening is
you point out that treatments over the last 50 years for cancer haven’t really come come along that far
there’s been certain / kind of exceptional cases lymphoma leukemia for example
but for the most part our overall survival rate from cancers is not much better than it was several decades ago
is that right
for metastatic solid organ cancers
so that does not include leukemias and lymphomas especially Hodgkin’s lymphoma
where we’ve had the field has had remarkable success
when you talk about / epithelial上皮の tumors solid organ tumors
it’s been an improvement in overall survival of five percent / in 50 years /
- Checkpoint inhibitors and other immunotherapy
now we’re starting to see those numbers get better and better with immunotherapy
and specifically a type of immunotherapy called checkpoint Inhibitors
so I think we’re probably getting to the point now where
maybe that number is getting closer to a 10 percent improvement over where we were
because approximately eight percent of all tumors today are now responsive to immunotherapy
and immunotherapy has the advantage of when it works
it is usually a very durable remission
meaning that remission tends to stay
it is effectively a cure
so of all the things that I think have come along in the past 20 years
I think immunotherapy is by far the most interesting part of cancer treatment
/ I was very fortunate in that just by luck that’s what I did
my research in so back as a medical student
/you know/ when I went over to the NCI the National Cancer Institute
I spent time working there and then I went back again for a fellowship more formally
/ when I was in residency
and the great pleasure of spending two years /you know/ working in the lab and doing that type of work
at the time it was pretty much exclusively a treatment for melanoma and
a little bit of a kidney cancer called renal cell carcinoma
but we were just starting to see the power of checkpoint Inhibitors which we used at the time in melanoma /
and today we realized that these checkpoint Inhibitors can work on any tumor
provided they have a certain type of mutation
now the goal is what does it take to create and unleash〔~を〕引き起こす the immune system on any type of cancer
how do you do this when we know
by the way
that 80 percent of solid organ cancers have cancer antigens that are recognized by the immune system
- Inside the body vs outside the body cancers
I want to talk about / each specific type of cancer screening that we have available that you recommend
and I think it’s helpful the way that you organize kind of the the two big buckets of cancer screening into cancers that happen inside the body and Cancers that happen outside the body
can you kind of go over that distinction
/ it is kind of funny because most people don’t think of their colon or their stomach is outside their body and
I understand why of course
but you have to think about it through the lens of embryology胎生学、発生学 right
you sort of develop in these multiple layers three layers to be specific
but the easiest way to think about it is
can the air that you breathe or that’s outside your body
can it get to the tumor
can it touch the tumor directly
so for example when you consider all of the skin cancers
the answer is yes right
your every everything on the outside of your body via vis-v your skin is exposed to the outside world
but what’s a little more / less intuitive is that
everything from your mouth to your anus is also technically outside your body
now the significance of this is primarily that you can look directly at it right
it’s that you can take a direct look at these cancers and
where it gets particularly noteworthy at least in the United States is that
colon cancer is the third leading cause of cancer death
so you have the number one being / lung cancer number two is kind of split between genders
so if you’re a man it’s prostate cancer
if you’re a woman it’s breast cancer and
then number three straight across the board is colon cancer
and interestingly colon cancer unlike the others that I mentioned lung
which by the way lung doesn’t occur in the air sac肺胞
so what I said about being able to look at it directly doesn’t really apply to lung
- The power of direct visualization of colon and polyps
/ but what’s amazing is that
you can look directly at the colon as it transitions from being perfectly normal to developing something called a polyp and that transition is a necessary first step towards the development of colon cancer
now most polyps do not become colon cancer
but every colon cancer comes from a polyp
this is a very important step means the development of a polyp is a necessary
but not sufficient step for the development of cancer
and we have a tool that allows us to look directly at the colon and identify any and all polyps and remove them
and if you think about that the implication is really
nobody should die of colon cancer
if we accept screening at a high enough rate
it should certainly be far less than it is today
it shouldn’t be the third leading cause of cancer death
it shouldn’t kill 50 000 people a year so
- Colon cancer screening specifics詳細: age, frequency, etc.?
on the topic of colon cancer
what age if someone were to visit you as a patient
what age do you recommend their first colonoscopy
and that’s assuming they’re willing to /you know/ pay out of pocket if needed for it
so it depends on number of things
it certainly depends on family history and
other personal risk factors such as /you know/ Crohn’s disease ulcerative colitis and things of that nature
but if we talk about a person who has no other risk factors and no family history
we still take a very aggressive posture and typically begin screening at 40.
which is five years ahead of the current recommendation
and 10 years ahead of the last recommendation
up until very recently the recommendation for first colonoscopy was 50
that has been reduced to 45 which I think is a very / good first step
when you consider how many people under the age of 50 were dying from colon cancer
and then the frequency I imagine also depends on what’s of course found in the colonoscopy
yes although again
here’s where we are much more aggressive
we typically recommend screening at no longer than every three years
but also depending on what’s found so if you find a certain type of polyp that is indeed
pre-cancerous we would screen much more frequently
- Bowel prep for colon importance and tips
it also depends on the adequacy with which the endoscopist was able to visualize the colon
so when you do a colonoscopy as anybody listening to this will recall you go through something called a bowel prep now fortunately /you know/ I’m 50 so I’ve already had three of these things
just in the last 10 years
the the bowel preps have become much much easier
in fact the last one I did a year ago was at walk in the park relative to the first one in terms of /you know/
I was able to do it using a product where you only take 12 or 24 pills over the course of a day
and you have a much easier bowel prep
but when the endoscopist is in there he or she basically makes a designation
it’s a scale it’s a rating system I believe it’s one to nine or zero to nine
I think it’s called the Boston bowel prep score or something to that effect
but it’s basically How well was I able to visualize the colon
and so we’re really looking for two things right
to wait three years to do it again we want no polyps and we want a perfect visualization of the colon
- Colonoscopy risks and upper endoscopy (Barrett’s esophagus)
and if those conditions aren’t met then we /you know/ decide on what colonoscopy should be
I would note that given that the biggest risks of colonoscopy are the bowel prep itself
which for people our age is not really a risk at all just an inconvenience
but for older people absolutely is a risk
there’s a risk of electrolyte abnormals and dehydration the sedation《医》鎮静剤の使用[作用] itself is a risk
again all of these risks are small but none of them are zero
so you have risks that are associated with /you know/ not breathing and things like that
and then finally there’s a risk of bleeding and perforation from the colonoscope
given that you’re having a colonoscopy you’re buying all of those risks
we generally recommend our patients undergo an upper endoscopy
so to look at the esophagus and the stomach as well
because cancer from the esophagus《解剖》食道 to the duoden/《医》十二指腸 while less common than cancer of the colon is still collectively a relatively high probability cancer when taken together from mouth to duoden/ and
therefore given that it poses no additional risk to the patient
given that they’ve all the risk is baked into the colonoscopy we generally recommend doing that as well
and surprisingly we do at times find pre-cancerous lesions in the esophagus in people who maybe only report /you know/ occasional heartburn for example which is a significant risk factor for something called Barrett’s esophagus which is a pre-cancer of the esophagus
and you recommend that upper endoscopy at every colonoscopy if one can get it
it depends /you know/
I can’t it’s impossible for me to take a blanket statement十把ひとからげの言い方
even though I’m sounding like I’m sort of doing it now
every case is different
/ but we’re basically asking that question with every colonoscopy
should we do the upper endoscopy at the same as well
- Pills for colon bowel prep (Sutab) vs liquid prep time
what was that product that you had such a wonderful bowel prep with
because my most recent colonoscopy was / that anything that would that /you know/ it wasn’t a great experience
/ the last one that I’ve done and now this is what most of our patients do
it’s called sutab I think it’s s-u-t-a-b and I think just basically twice the day before or like once the afternoon before and once /you know/ a couple hours before bed
you’re taking like 12 tablets with a large amount of water /you know/ probably 20 ounces of water or something like that
and yes it’s an infinitely more pleasant experience especially for people who don’t like the taste of a lot of these things which again going back 10 years ago when you were drinking something called Go Lightly
I mean that stuff was an Abomination嫌悪の対象 and the volume you had to consime was unbearable
I think that’s what I had was the Go Lightly
/ / they should ban that stuff
- Tips when choosing a GI specialist for a colonoscopy
you had some specific for people that haven’t had a colonoscopy before or /you know/ are willing to change their their endoscopist / or GI specialist what
what things should people be looking for in
/ /you know/ someone that’s going to do a perform a colonoscopy on them
/ I remember in the book you had some specific recommendations for things to look for
/ we have a whole bunch of recommendations in the book but I mean
I think some of the big ones are I just I would always ask your endoscopist what’s your perforation穿孔 rate
in other words it’s nice to tell me globally what the perforation rate is
but that’s a very misleading number because it also involves all sorts of patients
some of whom are very very sick
so the real question is an outpatient elective colonoscopy
what is your bleeding rate what is your perforation rate
I would also ask what is your SQL intubation rate so how often are you getting into the cecum/《解剖》盲腸 /
what is your typical endoscopy time so what is the total time of scope
- Blood tests for colon cancer screening (FOBT and Cologuard)
and I provide in the books of metrics on which you’re kind of looking for
what would be considered ideal for this purpose
great any other thoughts on colon cancer screening before we move on to perhaps
maybe breast and / prostate screening
/ I think the other thing I’d mention with that is that a really elegant thing to do on the off years of colonoscopy is to do a stool-based test
so you can do / like a fecal occult blood testふん便潜血検査 although that’s far less effective than the immunohistochemistry tests
so let’s just say you’re getting a colonoscopy every three or four years
if on the years you’re not doing it you’re doing a stool test that’s looking for tumor DNA /
you’re at least looking for a signal in those off years
now again that’s nowhere near as effective as a colonoscopy but of course it poses no risk
so it’s it’s in my mind kind of better than not doing anything in the off years
and if the stool test is positive then you would go straight to a colonoscopy
- How quickly can colon cancer develop?
okay yep because / you point out that despite maybe what people think colon cancer can develop in as little as six months in some patients right
/ it’s a big controversial / there have been case reports of that nature of course the alternative explanation for that is that that cancer was there six months earlier but somebody missed it so the truth of it is we actually don’t know what the time is to develop a colon cancer right
clearly it’s a way way way less than 10 years
so the idea that you would only do this every 10 years to me is absolutely insane
/ but /you know/ maybe it’s one year
maybe it’s two years
maybe it’s three years
we just don’t know / what what it is
/ and when we see those case reports it’s easy to be suspicious that
it’s not that you really developed a colon cancer in six months / but it’s possible that it was missed six months ago and either way it reinforces the need to be vigilant用心深い
and for the stool test is there one in particular that you tend to recommend more than others
I mean again it just comes kind of down to your budget but we probably like Colo guard the most
and I can’t even remember how much it costs
let me put it this way
they cost significantly less than getting a colonoscopy /
- Breast cancer: Peter Attia’s approach (age, modalities, etc.).
let’s talk about breast cancer and again maybe just start with your your approach
to breast cancer screening if there’s / /you know/ a particular age
I know every patient’s different but /
if there’s not a strong family history of breast cancer
is it a particular age that you recommend /you know/ starting screening for breast cancer
well again your breast cancer is pretty common
a woman’s lifetime risk of breast cancer at least in terms of having it not necessarily dying from it is is high enough that I think you have to approach every woman as though she’s at risk
and clearly family history here is a very valuable tool for at least a woman who has not been adopted right
so if you have a woman who’s not adopted and in whom we can look at her mom her grandmother both sides / her aunts on both sides
if we can start to get / some insights there that can really shape our thinking
so if we’re again let’s say dealing with somebody who does not have a family history of breast cancer
well I should say even more there’s more detail to it that I I think is kind of maybe beyond the scope of our discussion but there’s more Nuance around this right so sort of
if breast cancer occurred in family members
it’s also important to understand if it was pre or post menopause
so early life versus late life breast cancer kind of gives us a slightly different algorithm for how we screen
we then look at some other very personal factors for example a woman’s breast tissue how dense高密度の is it right
so the denser the breast tissue the greater the likelihood that you’re going to miss a breast cancer on screening
I think the most important thing and I want to just be clear like /you know/
there are people who for whom this is their specialty and
I would think that they’re far more knowledgeable about this than me
so I’m only talking about this through the lens of how we think about it with our patients
but /you know/ I think there’s no form of cancer screening where the idea of Stack 〔物を棚に〕並べる
stacking different modalities is more important than in the breast
- “Stacking” screening modalities for breast cancer
so to be clear I don’t think there is any single modality that is sufficient for screening breast cancer
every modality has a strength and weakness
and the good news is they are opposing
so for example mammography is very good at picking up calcified lesions
- Mammography strengths and weaknesses (dense breast tissue)
so lesions that have /you know/ little specks of calci/ in them and
certainly cancers can have little specks of calci/ in in them that tends to be later in life
so younger women don’t necessarily get as many calcific breast cancers ????
it also tends to struggle with dense breast tissue
so you’re going to get a lot of false negatives and a lot of false positives
frankly in a low prevalence / population of young women
- MRI and ultrasound for breast screening pros/cons.
conversely if you look at something like MRI
MRI has much more sensitivity to pick up breast cancer
although it actually has kind of low specificity and it tends to miss all calcified lesions unless they’re really really big
so it has an enormous blind spot to the very thing that mammography is very good at
and then ultrasound offers /you know/ advantages and disadvantages as well
so the first thing I would say is whenever you decide to start screening you have to be thinking about using at least two modalities
so I think mammogram should be an automatic for every woman and then
I think the question based on risk should be is ultrasound the right thing to do in concert with it
or should it be MRI and even within MRI there’s different ways to do it
so the gold standard would be something called multi-parametric MRI where you’re using contrast and something called diffusion weighted Imaging which I I think I explained in the book why that’s such a special tool to enhance MRI
- Stagger〔出来事などを重ならないよう〕調整する cancer screening modalities?
when you stack those modalities do you typically stagger them out
/you know/ maybe get a mammography test done one year
and then an MRI done the following year
or do you tend to get them at the same time and do they complement each other / / kind of in real time
great question / there’s no right answer to this / it depends on the patient
so for some patients we stagger everything by six months
so they’ll do an MRI every year and a mammogram every year
but they’ll be offset by six months
so they’re doing a form of screening every six months / that that would be kind of a higher risk woman
for other women you might do mammography every year an MRI every two years
so there’s an endless permutation配列 in here
and /you know/ again we don’t have level one evidence telling us what the right answer is but of course level one evidence don’t really apply to this type of screening for the reasons I talk about in the book which is
/you know/ level one evidence are also going to concern themselves with cost societal cost or cost of screening
- Level 1 medical evidence and costs
I think that’s a totally valid concern
but it’s not one that I concern myself or my patience with which is
we’re asking the question that’s slightly less constrained which is
if you ignore cost what is the right approach to screening
and there you only have to concern yourself with harm right
false positives psychological harm / and /you know/ opportunity cost but but
you don’t really need to think about monetary cost / which again
it’s important it absolutely matters at the societal level of somebody else is paying
but I I think it’s a personal choice for anybody who’s going to pay for themselves
- Genetic testing for breast cancer vs family history?
along those lines / genetic testing for / for genes that may increase the risk of breast cancer
do you typically recommend that
we do it in select厳選した[された] patients
so if the family history comes up completely Stone Cold 〔事実などが〕確かな、揺るぎないnegative
we typically do not do it /
if the if it comes up a little suspect we certainly do
obviously one of the genes everybody’s looking for is the the family of bracketひとくくり[まとめ]にする、一括する genes
/ usually it’s pretty obvious when that’s the case just from the family history
but you would absolutely want to confirm that genetically
/ but /you know/ the the real edge cases are the ones that are probably more interesting
which is not a bracket case which is usually quite obvious
but sort of a non-bracket case when there are other
unless /you know/ further from being deterministic決定論的な genes
and bracket by the way is not necessarily deterministic
but you have genes that are just more subtle increases in Risk
again there are reasons to do this both from an a financial perspective right
so once you have a gene that places you at greater risk obviously more of your care is covered
so that’s very important it also has significance in terms of /you know/
planning and expectations around having kids /you know/
if a woman has one of these genes she’s going to be much more on guard
/ if she has a child than can can sort of think through those things
and of course ultimately if the risk is significant enough a woman can elect to do something much more aggressive than screen which is to prophylactically予防的に undergo a mastectomy and just eliminate the source of the t/or but for a tumor forms
and interestingly there are a number of cases where women prophylactically do get mastectomies in breasts that otherwise appear normal only to find out~したところで~に気が付く that they actually do have microscopic Foci(focus《医》病巣の複数形) of tumor at the time of mastectomy
any other thoughts on breast cancer screening before we move on to prostate cancer screening
- Liquid biopsy for cancer detection
I think one other thing I would just say on breast cancer is the the other tool
that we do use here and it’s it’s a very emerging tool is that of the liquid biopsy
so liquid biopsies are still in their infancy初期段階
but they are already showing promise and breast cancer is an example where /
if you just look at the data superficially you would probably convince yourself that they’re not very helpful
but if you look at the data more deeply and I cite an example of this in the book
I think you start to realize that liquid biopsy becomes yet another tool that we should include in this
so superficially the data for early detection of breast cancer with / a test called The Gallery test by a company called Grail suggests that the sensitivity is very low
something on the order of 20 percent for stage one and stage two breast cancer
while the specificity is very high north of 99 about 99.5
so low sensitivity High specificity means if a tumor is there you might not see it
/ but if no tumor is there you’re going to get it right ?????
that’s effectively what that means well
again that doesn’t seem like it’s very helpful
if you’re trying to screen for a cancer but when you look more closely at the data
and you segregate分離する out the breast cancers by type
and you divide them between hormone positive and hormone negative
so in breast cancer a lot of the prognosis and treatment comes down to
whether the breast cancer is positive for estrogen and progesterone receptors and another receptor called her2 new
so if you look at the triple positive which is all three receptors positive versus the triple negatives you have a very different story
the ability of the liquid biopsy to detect the triple negative at an early tiny stage tumor is over three times higher than it is for the Triple positive
the implication here is the liquid biopsy is much better at detecting more aggressive tumors
and therefore it might suggest that the stage one stage two triple positive tumors aren’t going to kill you
if you catch them at that stage which you’re going to catch with other means because they aren’t spreading
these tests are looking for cell free DNA 《遺伝》無細胞DNA ?????whereas you are catching the more aggressive tumors because they’re already spreading by the time they’re stage two
so that’s just another wrinkle〈話〉新趣向、知恵、妙案、うまい考え that I think has to always be considered as we kind of think about how to incorporate liquid biopsies into this
and for people that are new to that term
/ the the gallery test that you mentioned
/ if someone wanted to get that test done where what’s the process of actually attaining that
/ it has to be ordered by a physician to my knowledge
I don’t believe that they do a direct consumer I could be wrong
I mean I have no affiliation with this company
/ so in our case /you know/ when we choose to order that we we are the ones that order that for our patients
and it’s a blood test so it’s a /you know/
it’s a test that takes two tubes of blood and returns a result in a relatively short period of time usually within two weeks or so
/ and you mentioned that it basically gives you information about a couple different things
-a do you have a cancer present potentially and
-B where is it coming from in the body
and you also mentioned maybe you could speak to this a bit that it’s
/ and correct me if I have this this right
that your opinion is it’s not a great just broad screening tool for cancer
it should be used / in general for for specific purposes or to stack with other screening modalities
/ I mean I would say that we do use it as a Pan cancer tool
but I’m generally not going to just rely on it by itself
so I’m not going to just say we’ll
we’ll do the test and if it comes back negative we don’t have to do anything else
/ I I just I don’t have enough confidence in any test to say that
including a whole body MRI
/ so I view everything as a stacking /you know/ optimization problem
- The future of liquid biopsies for cancer screening you see the technology advancing with the with liquid biopsies to the point
where /you know/ maybe we would be able to say with more confidence
I guess that what really needs to happen is the false positive rate would need to drop significantly on the test right
/ I mean I think we have to
I think the problem with liquid biopsies is is it
it’s a very important conceptual issue we have to wrap our heads around ~の周囲に[を回り込むように]配置する
which is what is a false negative what is a false positive
like what do they actually mean
because when a person gets an MRI or a mammogram or a colonoscopy
/ well let’s take colonoscopy out of it
so colonoscopy you are looking directly at something
there is no false positive right
there’s no false positives in colonoscopies
there’s false negatives if the bowel prep isn’t good or the endoscopus just missed it
but there’s no such thing as a false positive
but like if you’re looking at an MRI or a mammogram
a false positive means you’re looking at a set of pixels that are meant to represent something that is happening in the body that is an anatomic feature right
it is purely an anatomic test
a liquid biopsy is not an anatomic test
in some ways I don’t have a good word for it but it’s
it’s a biological test maybe right
it’s testing the ability of that cell to escape its primary location
such that it’s shedding抜け落ちる cell free DNA that we have to wrap our heads around
what that means and what the implications are for screening
and I don’t think we fully have yet and
that’s why I don’t think it will ever make sense to rely on a biological or functional assay機能分析 in exclusion排除、除外 of an anatomical assay or vice versa
I think we just want to come back to all of these things all of the time
because it also increases the Fidelity忠実性 of the test right
what we don’t want to do I mean we have to accept the fact that if we’re going to be aggressively screening
we’re going to find a lot of false positives
it’s impossible to have 100 sensitivity and 100 specificity
it’s impossible so you can plug those numbers into a spreadsheet and it will tell you that
for any prevalence of cancer even a cancer that only exists in one percent of the population
you’ll have a hundred percent positive predictive value
and a hundred percent negative predictive value meaning every time it’s positive it’s truly positive every time it’s negative it’s truly negative
but nothing comes close to that right
so MRI has almost a hundred percent sensitivity
but its specificity is abysmal 〈話〉非常に悪い、ひどい
liquid biopsy is the opposite
its specificity is almost a hundred percent its sensitivity is abysmal
now here’s the thing it is not the case that when you add two tests
you add their sensitivity and specificity so it’s mathematics behind that are more complicated
/ but clearly the more tests you add the more shots you’re getting on goal to pressure test耐圧[加圧・圧力]試験 what you’re seeing
- Metal detector analogy for sensitivity vs specificity
speaking of sensitivity and specificity
I like an analogy that you’ve used before of a medic a metal detector with regard to these tests
that they can I mean they can really be set however the the test makers want to / to set them
could you kind of explain that analogy and how it fits with liquid biopsies for example
sure so I’m sure people have experienced this all the time right it’s like
/you know/ you go to you’re passing through an airport metal detector and it goes off
and you think to yourself
dude I’m wearing the exact same thing I was wearing three days ago when I went to the metal detector at the other airport and it didn’t go off
how is that the case
like did I some did I somehow suddenly take on a whole bunch of metal
no the sensitivity of that metal detector has just been set to be higher or lower
depending on how you want to think about it
so in other words it’s it’s going to kick off at a lower threshold
okay so let’s now play the thought experiment right
so put yourself in the minds of TSA
so you get to set the sensitivity on the / on the device
you get to say what is a positive so sensitivity is the definition of the true positive rate
so if you set that thing to be very very Twitchy過敏な
the likelihood that anybody will get through who actually has metal is you can make that number exceedingly low
but what’s the problem with that the problem with
that is that most of the people going through who don’t have metal are still getting stopped
so /you know/ you basically create a log Jam渋滞 problem where you’re creating a whole bunch of distress for no reason
but In fairness no bad guys are getting through
conversely you can say all right fine fine fine
let’s set the bar really really high
so anyone that we catch is a bad guy and the /you know/ we’re not going to create any distress or false positive
but the problem is there’s absolutely going to be some bad guys that get through
so if you said it such that I’m going to catch anybody carrying an 18-inch knife or a gun
that’s fine but maybe somebody walking through with /you know/ a six inch knife isn’t doesn’t have enough metal to trigger it
so that’s basically as you say kind of the decision everybody has to make as they work through how to tune a screening test
are you tuning it more towards no false positives or more towards no false negatives
and sometimes that’s the nature of the test
so for example an MRI because of the resolution that it can produce
it’s generally geared towards higher sensitivity
it’s going to overcall things
especially in glandular tissue like the thyroid gland and the pancreas and things like that
but in a liquid biopsy it’s a hundred percent at the discretion of the scientists as they tune the algorithm
- Prostate cancer: Dr. Attia’s approach to PSA, imaging, and 4K tests
makes sense okay getting back to prostate cancer screening
/ this is one that /you know/ most people watching this have heard the PSA test for for prostate
but could you explain what PSA is and how we can do better than just look at at the PSA number alone for prostate screening
so PSA stands for prostate specific antigen and it’s a protein that is made or an antigen that’s made by cells in the prostate
and obviously it’s not made by other cells that’s why it’s prostate specific
and the value this this this is a biomarker that you can measure in the blood
and this value is proportional to the size of the prostate gland but it also comes out disproportionately when a person has prostate cancer
so we tend to think of the prostate in either /you know/ milliliters or grams
we can estimate the size of it pretty well on an ultrasounder on an MRI
so if you took two people who had the same size prostate
so let’s say a 25 gram prostate which is a normal size prostate
/ /you know/ you would expect them both to have a relatively low PSA
/you know/ probably at or below one let’s just say it’s one
but if one of those people all of a sudden has a PSA of four or five
even though his prostate isn’t significantly larger
you would certainly be worried about the risk of prostate cancer
because again once those cells make the transition to becoming cancer cells
they’re going to secrete more and more of this prostate specific antigen and
historically prostate specific antigen or PSA was a screening test that was done for men /
it was always one that created a lot of consternation驚愕、仰天 within the community because it was a test that when used by itself had a lot of false positives and frankly a lot of false negatives
so false positives meant there were a lot of men who were /you know/ showing up with a PSA value that was higher than you would have expected based on /you know/ their age for example
and the next step was to do a biopsy of their prostate gland to make sure they didn’t have cancer
and lo and behold they wouldn’t have cancer and you you just subjected them to a pretty aggressive procedure
/ /you know/ a trans rectal biopsy of the prostate is not a benign procedure
/ not having had one
but certainly having spoken to many people who have I’ve never heard anybody say that was pleasant
so / and not without complications by the way
so so the question is how could you make the predictive value of the PSA better this
by the way is another question of where do you set the bar
so let’s go back and think about this through the lens of your metal detector
you could say we are not going to biopsy anybody below a PSA of 10.
and if that’s the case outside of guys with prostatitis
you’re only going to be biopsying people with cancer
but you’re going to miss a lot of people with cancer too
you’re not going to have false positives you’re going to a lot of false negatives
if you say okay we’re going to biopsy everybody who’s over three
oh my God you’re probably not going to miss many cancers
but there’s a lot of people getting biopsies who shouldn’t get them
so today what we do is we don’t just look at the PSA
we look at several other metrics
we look at something called free PSA which is the percent of PSA that is Unbound
it’s not being bound to other carrier proteins
and so the percent free also gives us a clue as to whether or not this is a prostate cancer or not
we look at something called PSA density which is the PSA value normalized to the size of the prostate
we look at something called PSA velocity which is the rate of change of PSA value over time
all of these things so higher PSA velocities /higher PSA densities /differences in percent free PSA add color 彩りを添える[与える]Beyond just PSA and will /you know/ give us a much earlier indication早期表示する as to に関してwhether something is significant in which case we can depending on the PSA value either move to another type of blood test called a 4K test which is kind of like another liquid biopsy for prostate but it’s specific to prostate
- Multiparametric多重パラメーター MRI for prostate screening
or move directly to a multi-parametric MRI which is very similar to that multi-parametric MRI I talked about for breast tissue where you’re looking at these different types of pictures so different types of images of the MRI T1 T2 diffusion weighted Imaging Etc with and without contrast 7
so where we basically are now is very few men are undergoing unnecessary biopsies
in fact I don’t think in the last 10 years
I’ve had a single patient undergo a prostate biopsy that did not find cancer
so the implication is by the time we’re sending a patient for a biopsy today, we know he has cancer
it’s just a question of how aggressive
now some of those men come back with a cancer that is not very aggressive
and the collective decision of the urologist and the patient is to wait a year in biopsy again
and in one of those cases I can /you know/ I just think about a patient very recently
there was enough of a change in the histology《生物》組織学 over a year
that they said enough is enough we’re going to do surgery now
in other cases the answer is let’s wait another year and do it
/ and or compare it to /you know/ other characteristics of the MRI
so the point is /you know/ this has largely become an issue where we are less /you know/ doing these biopsies with low probability / you know/ thinking in terms of outcomes
these additional PSA blood tests that can be done
the PSA velocity/ density and free PSA / or what was it the 4K / and then the 4K as well
well so the so when you order a PSA test, a lab will typically default into a free PSA
they’ll reflex a free PSA test if it’s over three typically
so I don’t I forget is it three or four but usually with a high enough PSA I think over three
you can automatically just get the free PSA
the other ones you actually have to manually calculate
the lab won’t tell you the density
you have to have had an ultrasound or some other Imaging of the prostate to know its size to
then calculate the prostate density
and similarly you have to keep track of the PSA values and plug them into
they have online calculators that’ll do this for you where you put in historical PSA data with time
and it will tell you the PSA velocity
got it
so that gets that my next question is I know this is something that you do at your practice with your patients
are any of these additional parameters Beyond just this
the simple PSA test mainstream in Family Medicine 家庭医療clinics across the United States for example to your knowledge or is this
it’s a good question
I mean unfortunately we know that there are lots of people who are falling through the cracks
so / you know/ someone who works with me actually
meaning one of my colleagues his dad was at his doctor and /you know/
he had a PSA level and it wasn’t particularly alarming
and his doctor wasn’t concerned
and the colleague of mine said well let me do a double check on that and ran it through the PSA velocity check and actually the PSA velocity was higher than 0.45
so that’s generally the cutoff meaning anything that’s growing more than 0.5 the units aren’t important
but 0.5 /you know/ 0.45 units per year anything that’s growing at a rate beyond that is alarming
and even though the absolute value of his PSA wasn’t that high the velocity was
and so he went back to his dad and said hey you need to go and get more testing done
you probably need a biopsy or at least an MRI
and his doctor said no he doesn’t /you know/ this is totally fine
and so /you know/ this colleague of mine just told his dad /we’re going to go around your Dock and just go and pay and get an MRI
they did the MRI indeed showed that he had a cancer
he got a biopsy he was cancer he’s already had his prostate taken out
wow / so /you know/ his son saved his life
/ and it’s disappointing that the doctor was completely unwilling to even acknowledge this
/ so /you know/ I’m guessing /if that happened once it’s going to happen a few times and
- Empowering ourselves as patients with knowledge
unfortunately I think what the lesson is there is, you as the patient probably have to be the owner of this process and you really can’t rely on anybody else
now / I think that particular doctor had an arrogance about him that’s sort of deplorable嘆かわしい
/ but the reality of it is
even a well-meaning〔人の言動が良い結果を生まなかったが〕善意の(ある)[から出た] doctor
I think can miss something or maybe just isn’t keeping up with this literature
so I think /you know/ everybody has to kind of take ownership over this problem for themselves, which is unfortunate because in an ideal world that’s why /you know/ I shouldn’t have to take ownership of my car when I take it to a mechanic
that’s why I’m taking it to a mechanic / but unfortunately I think /you know/ that might be the case
- Incidence of prostate cancer. 80% in men of age 80?
how common is prostate cancer in men and /you know/ I think many watching this have heard
that many people die with prostate cancer not necessarily from it
so how do you explain the overall risk of prostate cancer to your patients
/ no I think that’s exactly what I say is
virtually every man will die with it fortunately not too many die from it
but it is still the second leading cause of cancer death in a man only behind lung cancer
so /you know/ it’s not a particularly lethal cancer compared to say pancreatic cancer
or /you know/ certain types of brain cancer or lung cancer
I mean those are incredibly lethal meaning once you get
it you’re very likely to die that’s not the case with prostate cancer
but because so many men get it
and even though the lethality is not that high the absolute numbers are pretty devastating
the thing about covid right
virtually nobody who got coveted died of it but
because everybody got it the total death toll actually was pretty high
- Lung Cancer increasing in never smokers
you mentioned lung cancer there being the number one killer we know
it’s a huge risk for for people that smoke
but what is the risk for people that don’t have never smoked
/ sadly it’s not zero right so 15 of people who develop lung cancer are never smokers and
/ sadly we see that disproportionately in women over men and we see that women non-smokers are the fastest segment of cancer of lung cancer growth
that’s again that’s a very sobering酔いも覚めるような、ハッとするような statistic for which we have no great explanation
I wrote an article on this /you know/ on in our blog newsletter several months ago
if people are interested they can go back I mean /
Catherine who’s the analyst that I worked on this with / you know/
I think we went kind of back and forth on some of the whys /you know/
is it something to do with estrogen
is it something to do with /you know/ different types of gases that women might be more exposed to
I mean the short answer is I don’t think we really have a great answer
there’s clearly some difference / either genetic or otherwise that is pointing to this susceptibility that non-smoking women appear to have and /
and again they disproportionately 偏って
it’s an adenocarcinoma of the lung that is afflicting them and it’s very frightening because
again nobody’s thinking about lung cancer screening in a non-smoker
it wouldn’t cross your mind to take a healthy 40 year old woman who’s never smoked and Screen her for lung cancer
that’s just the furthest thing from your mind and
we have a patient who / has survived an aggressive adenocarcinoma of the lung
only because she was so lucky in that ~という点においてshe had a CT a calci/ scan
a CT a special CT of the heart to look for calcification in the heart
and it just happened to pick up a small cancer
and I think had that cancer been caught a year later / you know/ I think / there’s a good chance it would have been too late
- Full body MRI screening for cancer?
this kind of ties in with lung cancer potentially you mentioned
/ earlier MRI screening for cancer taking someone who doesn’t have signs or symptoms of cancer and putting them on an MRI scanner using a special technique that you mentioned diffusion weighted Imaging 拡散強調画像
can you explain your recommendations around that to your patients
/ the value that you see in that type of screening
so again MRI is /you know/ has its strengths and its weaknesses
and its greatest strengths are it has no radiation so pose no harm to the to the individual unlike say a CAT scan or a pet scan which have tons of radiation and should never be used for General screening purposes with one exception that we can talk about later /
and it has a very very high sensitivity meaning if a cancer is there an MRI is pretty likely to see it
now there’s things that’ll miss this is only within the types of cancers that it can see
it’s not great for any of those outside the body cancers
so by the time a MRI is picking up a colon cancer or an esophageal cancer,
it should have been picked up years ago on an endoscopy
so you do not want to rely on this for diagnosing cervical cancer or endometrial《解剖》子宮内膜の cancer where you can that’s those are other examples by the way of outside the body cancers right
you can look directly at the cervix directly at the uterus Etc
so anything that can be looked at outside the body we’re going to do that
but if you take away those cancers / it’s a high sensitivity test but
it’s a very low specificity test meaning it’s just not good at differentiating
between Cancer and non-cancer in certain tissues namely glandular tissue《解剖》腺組織
so again MRI is the metal detector that’s beeping all the freaking time
it just doesn’t stop beeping
it’s the most annoying metal detector you’re ever going to see
so you’re stopping a whole lot of people that are posing no threat to the airplane
so in an effort to make that better,
a technique that was developed to look at Strokes is now being applied to the whole body
this technique is known as diffusion weighted Imaging with background subtraction but we just abbreviate it to DWI
what this technique does and it’s I will not explain this in great detail
because to do so I would actually need to explain how MRIs work and how the pulsing of the magnets makes protons move
and I honestly just think most people don’t want to get into that level of detail
but if you sort of just try to suspend disbelief for a moment
the way an MRI is basically working by detecting the movement of protons
that’s effectively what an mri’s schtick is
so a CT scan totally different stick right
a CT scan is shining electrons through something
and on the back side of that thing it’s collecting how many electrons hit it and
it’s imputing the density of the thing it went through based on the collection of electrons
MRI totally different
it’s power using powerful very powerful magnets and making protons move and
depending on how it pulses the protons, it’s measuring different aspects of the movement of protons
so protons of course are ubiquitous至る所[広くあちこち]に存在する in fat and water
proton is hydrogen right
so H2O and the CH group in a fat molecule
so we’re full of protons
it’s /you know/ most ubiquitous atom in our body
and the diffusion weighted Imaging trick is to pulse water and basically look to see how long it takes to move again and this works really well to determine how firm a piece of tissue is
so in the brain when a person’s potentially had a stroke
you can take a look and see the firmness of the tissue
even if there’s no bleeding in the area
now this works in the brain because the head doesn’t move
the head is the easiest thing to stabilize in an MRI scanner
and so the frequency with which they would ping these things was typically /you know/ 50 microseconds and that was quick enough that they could still see the artifact or the movement
to do that in the body is much harder
50 microseconds is not fast enough to actually get a good signal in the body
because you can’t limit the movement of the body as much
the body won’t stay as still as the head
so there are companies that are working on using faster and faster software to get that time down to 20 and even 10 microseconds
and at that rate the diffusion weighted Imaging is starting to work pretty well in the body
and it’s you can sort of think of it as a visual lump detector
it’s able to concentrate the signal/ the darkness of the digital signal around the firmness of the tissue
and that is serving as an effective way/one effective way to increase the specificity of an otherwise High sensitivity low specificity test
well I’ll reveal that I am thankful for this technology
because that’s what actually caught my cancer that caught my Hodgkin lymphoma company called pernuvo
/I know/ is offering them are they /the only one right now that offers the full body screening for for this purpose
pronuvo is probably the best MRI today at doing this detection now
there are other companies that do it but they’re just used like they’re licensing the pernuvo technology
but / at this time we are only having our patients get scanned in a pernuvo scanner either at pronuvo or at a facility that uses a pronuvo scanner
and hopefully someday insurance will cover this type of of screening because
as you mentioned there’s potentially a lot of value in it
but right now as far as you know/ this has to be out of pocket for it for probably
100 out of pocket / and what I tell patients is
don’t do this if you’re not willing to deal with the very high probability that something will be found
that is not cancer but will require additional work
- Aneurysm動脈瘤 on MRI
/ so /you know/ I I don’t have the exact numbers but it /I would say/ at least 20 percent of the time
we send a patient for one of these scans
we /you know/ get the news that / there’s almost assuredly nothing here but there’s this other thing
there’s this potential and by the way sometimes these are important things like you catch aneurysms that /you know/ an aneurysm in the brain or in the pancreas can be lethal if not caught
so sometimes you catch these other things and you go ahead and you fix them
so all comers were seeing /you know/ about a point seven percent aneurysm catch rate now
probably a number of those will go on to be just fine if you did nothing about them
but a subset of those have lethal potential
but more likely you’re catching these kind of clinically insignificant other artifacts that you do need to Chase and pursue
and as a result of that I don’t know /I would say/ maybe 15 of our patients just elect not to do a whole body MRI for that reason which is they just they don’t feel like their constitution気質、体格、体質 is gonna /you know/ deal well with the following months of uncertainty as these other things are chased down
and so I think that’s a wise and informed decision for them
and I think that’s that I just want to make sure
we don’t get to the point where people are doing this type of screening without having that discussion and nderstanding that hey /you know/ there’s a chance we’re going down a rabbit hole here
if you’re not ready to go down that rabbit hole don’t get on the ride
- Exercise and cancer prevention? / okay shifting to and you already mentioned this briefly
but / you mentioned cancer is probably the least well understood as far as what we can do to prevent it
/ but you also mentioned that exercise is perhaps the greatest longevity drug
/ so do we do /we have / evidence at this time that exercise can help prevent cancer
/ and that’s decoupling exercise from /you know/ the benefits it might have on someone’s / you know/ weight
/ if /you know/ taking someone from obese to to not obese
I mean we know that that can be helpful for cancer
but just can exercise alone help prevent cancer to our knowledge
/ I think it /I think there’s very good evidence that it can right
when you think about some of the things that exercise is doing so
so if you think about the metabolic benefits of exercise
/ it’s certainly far transcends weight loss
/you know/ muscle is by far the most important sink for glucose and so
insulin sensitive muscles are equivalent to insulin sensitive people
you can’t be insulin sensitive without having insulin sensitive muscles
you can’t have insulin sensitive muscles without exercising once you reach a certain age
I mean /you know/ a youngster maybe but
but certainly by the time you’re in your 20s and 30s, you have to be exercising to maintain insulin true insulin sensitivity and that may be the single most important factor there is
but going beyond that /you know/ exercise does a lot of things right
it creates a lot of myokines《生化学》ミオキナーゼ
a lot of chemical signals that do various things throughout the body including reducing chronic inflammation
and I think chronic inflammation is one of the impediments障害 of the immune system
and so if being insulin sensitive cuts down on the growth factors having less inflammation enhances the immune system and you could certainly make the case
and I would make the case that those are probably two of the most important things at our disposal when it comes to reducing our risk of cancer
- Possible impact of stress, immunity decline, etc.
excellent
any other cancer prevention strategies besides the ones that you’ve already highlighted that
that one should consider of course avoiding detrimental有害な things like smoking aside
/ I think those are really the big ones I mean there’s things we don’t understand /you know/ we probably don’t understand exactly the role that stress is playing on cancer
but I just have to think that there is a legitimate risk there through the the mediation介在 of hyper-cortisolemia 高コルチゾールand excessive gluco-corticoids糖質コルチコイド on the immune system as well so
so I think /you know/ just some level of immune system and immune cell exhaustion as we age is probably equally responsible for the exponential increase[指数関数的]増加 in cancer as we age
right I mean part of that I think is more time to accumulate mutations
and mutations are the core thing that are driving cancer
but I also think at least half of the equation is that our immune system is getting weaker as we age
and that’s actually one of the things where /you know/ if I think about all of the Sci-Fi things that are going on out there the one that I would most want to see come to fruition / would be /you know/ addressing the exhaustion of the immune system
so if we could sort of manipulate the epigenome of T cells specifically and turn old T cells into younger T cells again that that would have a profound impact I believe on cancer treatment
- Other cancer screening: cystoscopy, lung, more.
any other cancer screening modalitiesモダリティ
that we we missed we we talked about lung colon breast prostate
/ you mentioned screening for cervical cancer briefly /skin checks you mentioned any other any other ones that were missing that we have the opportunity to screen for
/ I mean there there certainly are and it’s always going to be Case by case right
so for example in a person with a history or a family history of bladder cancer
or in someone who has a personal history of smoking where /you know/ we would even recommend cystoscopy《医》膀胱鏡検査(法)
/ for people who are former smokers we also add low dose CT scan to the lung MRI
the MRI of the lung is with diffusion weighted Imaging is equal probably to the low dose CT for adenocarcinoma
but when you’re talking about small cell carcinoma /squamous扁平上皮 cell carcinoma or large cell which are more common in smokers I think you’re getting more benefit from the low-dose CT scan
so we’re doing a low-dose CT of the chest annually in former smokers as well
- Genetic testing for recommended? and then what about just genetic testing for your patients getting their their whole genome sequenced with something like 23andMe or one of those companies
I mean I think every one of these things has its place but they they you have to know what you’re kind of looking for before you do it
I mean again if a person’s been adopted養子縁組された then I think there might be some benefit in doing it
you might come up with something that you really didn’t know
but you’d be amazed what a very thorough family history can accomplish for a person
and / at least when it comes to cancer / you know/
I think we get we probably get more insight genetic testing on on some of the other diseases
- Final thoughts on EARLY cancer screening and the future
but / with cancer at this point in time we generally don’t routinely screen
and we use the screening selectively based on an individual’s history
okay well to finish up any other final thoughts on cancer screening or or prevention no I think unfortunately
/you know/ prevention and screening have to be our main strategies today
I think the the treatment landscape is / you know/ still kind of lacking relative to cardiovascular disease
though it’s further ahead than neurodegenerative disease
/ but /you know/ personally I remain incredibly optimistic about what’s going to come as far as /you know/ expanding the capacity of immunotherapy
again I said something at earlier that
that might have gone over some people’s heads because I just sort of mentioned it in passing〈文〉〔話の〕ついでに
but we now know that 80 of solid organ tumors have novel neoantigens新抗原 /meaning 80 of the cancers that people think about /when they think about getting cancers that kill /have enough antigen /that a person’s own immune system can recognize it
the problem is not enough of the immune cell can recognize it and that’s why ultimately the cancer wins
so we’re playing a game of tug and War綱引き、主導権争い right now
and the good news is we at least have some guys that can hold on to the Rope
the problem is we don’t have enough in most cases
so we have to figure out a way to increase the number of cells
the number of T cells that can expand to meet that need once they recognize a cancer cell
because I do believe that ultimately there is no therapy that’s going to rival that of immunotherapy
well Dr Tia thanks so much for your time



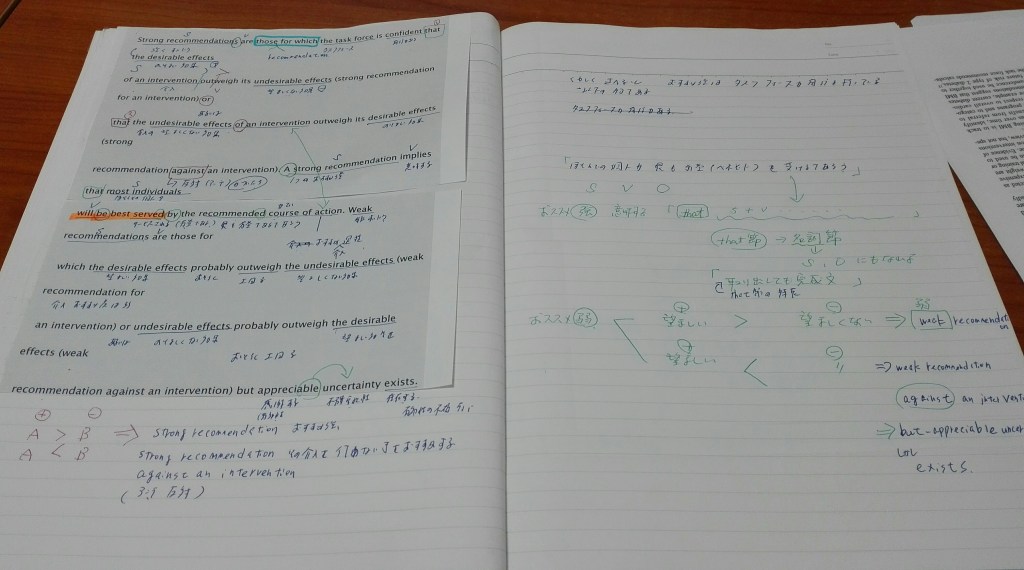
コメントを残す